|
The National Emergency Medicine Programme Model of Care
The Health Service Executive (HSE) and the Royal College of Surgeons in Ireland (RCSI) jointly launched the National Clinical Programme for Emergency Medicine Model of Care 2025 in September. This is the most significant update to Ireland’s strategy for delivering urgent and emergency care in more than a decade and highlights a shift towards more proactive and patient-centred approaches to urgent and emergency care and emphasises the importance of “right care, right place, right time”.
The Health Service Executive (HSE) and the Royal College of Surgeons in Ireland (RCSI) jointly launched the National Clinical Programme for Emergency Medicine Model of Care 2025 in September. This is the most significant update to Ireland’s strategy for delivering urgent and emergency care in more than a decade and highlights a shift towards more proactive and patient-centred approaches to urgent and emergency care and emphasises the importance of “right care, right place, right time”.
The document describes how multidisciplinary teams will play a greater role in delivering care, supported by expanded advanced practice roles and sustainable workforce planning and the importance of data-driven tools and digital innovation in to improving patient flow, guiding decision-making and supporting value-based care.
Minister for Health Jennifer Carroll MacNeill said: “This Model of Care is a comprehensive and welcome step forward to our shared objective of improving the quality, safety and accessibility of our emergency care services. At its heart, this is about dignity, safety and trust.
“Today, we are not simply launching a document – we are reaffirming our commitment to every person who attends an emergency department or injury unit, day or night. I want to sincerely thank the clinicians, nurses, healthcare professionals and patients who contributed to this model. Your unwavering commitment to excellence and best practice has brought us to this moment.
“As Minister for Health, one of my priorities is ensuring that people can access the support they need when they need it. I look forward to continuing the strong collaboration with the Emergency Medicine Programme as we work together to deliver better outcomes for all.”
|
|
Emergency Medicine Sustainability
In October 2025, the Health Service Executive (HSE) Climate Action and Sustainability Office and the Emergency Medicine Programme celebrated a major milestone in healthcare sustainability, as four Irish Emergency Care sites have now achieved Bronze status in the Royal College of Emergency Medicine’s (RCEM) GreenED Programme.

In October 2025, the Health Service Executive (HSE) Climate Action and Sustainability Office and the Emergency Medicine Programme celebrated a major milestone in healthcare sustainability, as four Irish Emergency Care sites have now achieved Bronze status in the Royal College of Emergency Medicine’s (RCEM) GreenED Programme.
This achievement marks the successful progression of the Green Emergency Medicine initiative, launched in partnership with the Health Service Executive (HSE) Climate Action and Sustainability Office and the National Clinical Programme for Emergency Medicine in Royal College of Surgeons in Ireland (RCSI). Supported by SPARK Innovation Funding, the project demonstrates the HSE’s commitment to reducing healthcare’s environmental footprint while maintaining the highest standards of patient care.
The four participating sites – University Hospital Waterford, University Hospital Galway, Mayo University Hospital and Bantry Injury Unit – have completed Phase I of the GreenED accreditation programme, implementing practical measures to reduce the environmental impact of Emergency Department (ED) and Injury Unit (IU) operations while maintaining or improving standards of patient care.
The GreenED framework, developed by RCEM, empowers ED staff to lead sustainability improvements within their departments, even in high-pressure clinical environments. Through this programme, staff have introduced targeted interventions to reduce energy use, waste and emissions, while maintaining safety, efficiency and quality of care.
Key outcomes of this project include:
- Carbon Measurement and Reduction: Using RCEM’s GreenED carbon calculators, teams measured and began reducing emissions from heating, lighting and medical supplies.
- Collaborative Action: Multidisciplinary staff at each site engaged in locally led interventions guided by the GreenED framework.
- Education and Knowledge Sharing: An eLearning module, informed by the experiences of these pilot sites, is in development to support other EDs and IUs in starting their sustainability journeys.
The success of these four sites demonstrates the scalability and impact of the approach and represents an important step toward embedding environmental sustainability into emergency care across Ireland. Seven additional sites will take part in the RCEM Green ED programme in 2026 bringing the total to 11 sites on an accreditation journey.
In addition, the National Clinical Programme in Emergency Medicine have launched the Green Emergency Medicine Guide” : a national quality improvement framework supporting Emergency Departments, Injury Units and Urgent Care Centres to start their sustainability journey. The framework sets out a scalable approach using a tiered structure of Must Do, Should Do and Could Do interventions and lays the groundwork for sites to progress towards the RCEM accreditation journey.
|
|
Emergency Medicine Airway Registry Ireland Preliminary Report
Launched with the Model of Care in September, the Emergency Medicine Airway Registry Ireland Preliminary Report comprehensive report on emergency intubation practices, patient outcomes and benchmarking across Irish hospitals.
The aim of the Emergency Medicine Airways Registry Ireland (EMARI) is to assess the practice of endotracheal intubation in Irish EDs. This will provide a local, regional and national overview of emergency airway management to audit and therefore improve the quality of care delivered to continuously improve patient outcomes. The airway registry will allow for the assessment of standards at a national level, with the additional benefit of enhancing national clinical guidelines.
NCCA and NOCA have confirmed support for the implementation of the Emergency Medicine Airway Registry of Ireland audit in 2025 and Zita McCrea (zitamccrea@noca.ie) has been appointed as project manager.
|
|
Emergency Care Activity Profile (EC-AP)
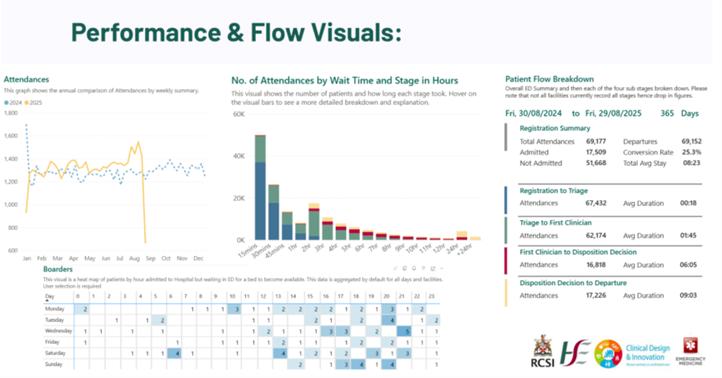
The Emergency Care Activity & Profile (EC-AP) dashboard is a tool developed by the HSE Integrated Information Service (IIS) and the Emergency Medicine Programme (EMP) to support Emergency Departments (EDs) with relevant clinical and managerial data.
The Emergency Care Activity & Profile (EC-AP) dashboard is a tool developed by the HSE Integrated Information Service (IIS) and the Emergency Medicine Programme (EMP) to support Emergency Departments (EDs) with relevant clinical and managerial data.
The system (described here) can display close to real-time information about the activity in the ED and compare it to the national average. It can also provide this information for time periods specified by the user and compare “like with like”, e.g. average attendances on a particular day of each week.
Focus this year has been on developing a robust process for allowing relevant staff access to the dashboard. The next stage of the project is the expansion of data to cover Injury Units and allow additional data availability which will include ED resources and issues log for each ED and IU.
The system allows staff to make best use of the data and streamline accessibility processes. If you are interested in becoming an EC-AP champion at your ED site or would like to access the EC-AP database, please contact emp@rsci.ie
The Open Door: Exploring Mental Health Emergency Care in Ireland
On 10 December 2025, the Emergency Medicine Programme (EMP) hosted The Open Door: Exploring Mental Health Emergency Care in Ireland at the RCSI Mercer Building, bringing together a diverse group of leaders and frontline professionals from emergency, mental health, acute hospital, community, research and policy settings.
On 10 December 2025, the Emergency Medicine Programme (EMP) hosted The Open Door: Exploring Mental Health Emergency Care in Ireland at the RCSI Mercer Building, bringing together a diverse group of leaders and frontline professionals from emergency, mental health, acute hospital, community, research and policy settings. The event created a dynamic and collaborative space to reflect on how Ireland responds to people in mental health crisis and how that response must evolve.
Across presentations, breakout discussions and design workshops, attendees explored the latest evidence on the rising numbers of mental health presentations to emergency departments. Contributors from patient representatives, the Mental Health Commission and the National Clinical Programme for Self-Harm and Suicide-Related Ideation shared key insights into national trends, system pressures and the lived realities that shape crisis care.
A major theme throughout the day was the critical interface between EDs, acute hospitals and community mental health services. Case studies highlighting children’s pathways and community crisis responses demonstrated both promising innovations and areas where fragmentation continues to impact care.
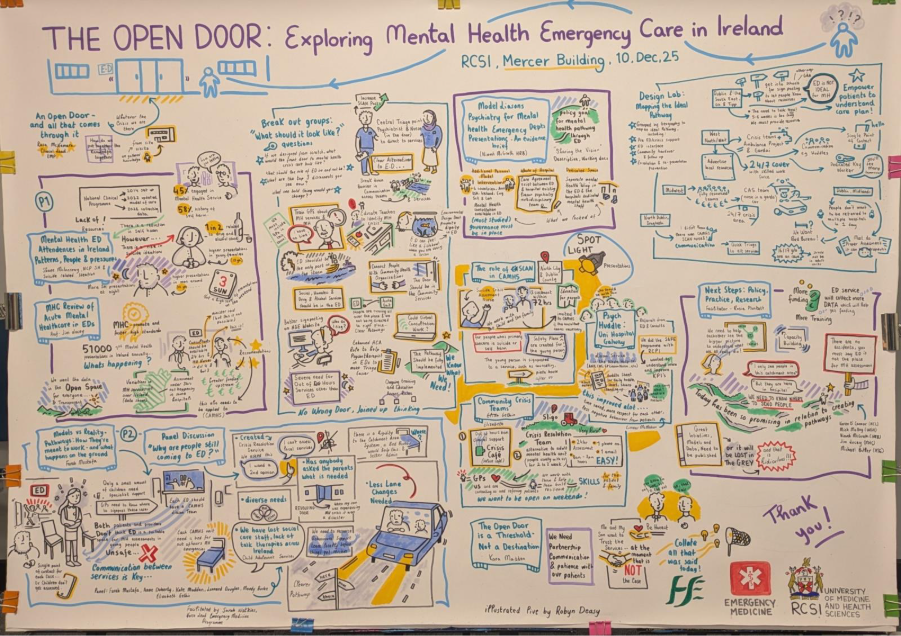
*Illustrated by Robyn Deasy
Injury Units
Since their establishment in 2012, Injury Units (IUs) have become a vital bridge between hospitals and local communities, providing timely and quality care. Attendance at IUs increased by 14.6% in 2024/2025, reflecting their growing importance, with plans underway to expand from 14 to 21 units by 2026.
Since their establishment in 2012, Injury Units (IUs) have become a vital bridge between hospitals and local communities, providing timely and quality care. Attendance at IUs increased by 14.6% in 2024/2025, reflecting their growing importance, with plans underway to expand from 14 to 21 units by 2026.
A key focus for improving IU patient care is strengthening multidisciplinary teams and enhancing staff expertise. To support this, the EMP has launched two initiatives: the development of an NFQ Level 8 Special Purpose Award in IU Nursing and research into the role of Advanced Practice Physiotherapists (APPs) in Urgent and Emergency Care (UEC) settings.
Meanwhile, the HSCP office has initiated a scoping review to explore the role of Advanced Practice Physiotherapist (APPs), who internationally have been shown to reduce patient wait times, length of stay and re-presentations while improving patient satisfaction. A pilot program will launch in Nenagh, Mercy and Our Lady of Lourdes Hospitals to assess APP-led care in the Irish context in IUs.
Collaboration across multiple stakeholders, including the HSE, RCSI, University of Limerick and international partners, ensures these initiatives are evidence-based and tailored to service needs.
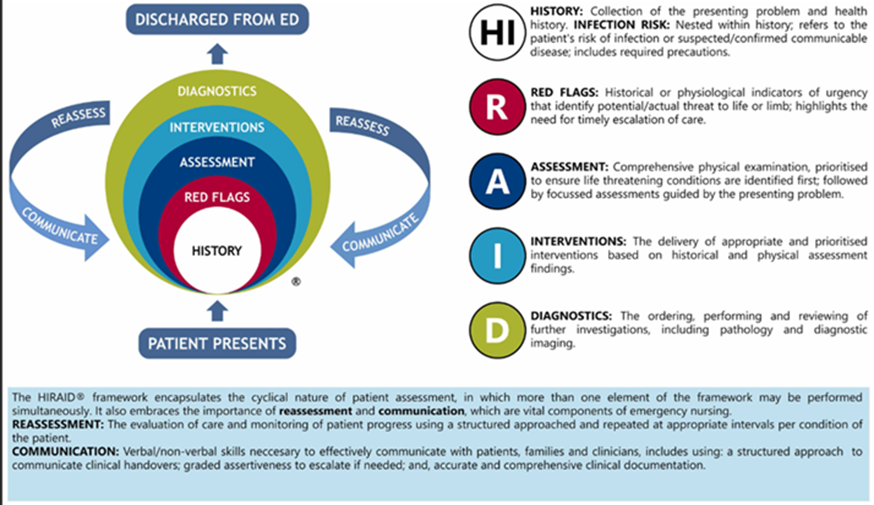
HIRAID: History (including infection risk), Identify Red Flags, Assessment, Interventions, Diagnostics, Reassessment and Communication
In October 2025, RCSI welcomed Professor Julie Considine Deakin Distinguished Professor and Chair in Nursing at Eastern Health Australia. Julie hosted a Seminar to introduce the HIRAID Emergency Department (ED) nursing assessment framework. The framework was developed by Julie and her team of emergency nursing experts and is the only validated framework to support ED nurses to assess and manage undifferentiated and undiagnosed patients after Triage. The Seminar provided an opportunity to explore and discuss the feasibility of HIRAID in an Irish nursing context.
Activity Based Funding
In last year’s newsletter, we explained the benefits of assigning an ICD 10 code to each patient attendance at an ED or Injury Unit and the important role that it plays in assigning an Urgency Related Grouper, for the purposes of Activity Based Funding, to each attendance.
In last year’s newsletter, we explained the benefits of assigning an ICD 10 code to each patient attendance at an ED or Injury Unit and the important role that it plays in assigning an Urgency Related Grouper, for the purposes of Activity Based Funding, to each attendance. This will mean that, for the first time, the ED phase of care will receive specific funding, in contrast to the current situation where block funding does not recognise individual ED attendances and the ED phase of care prior to admission, for those patients admitted to an inpatient bed, is not funded separately.
The diagram shows the five data points required for each patient attendance to allow that attendance be allocated to 1 of 114 Urgency Related Groupers (URGs). The URG, in combination with a parallel exercise in patient level costing for each hospital, is the means by which funding is allocated for each patient attendance.
The first four pieces of data are already returned from each hospital to the Business Information Unit as part of the PET return. If any of the five pieces of data is missing, the attendance will be assigned to an error URG, which means the unit will only receive a fraction of the funding for the attendance that it would have received had all five pieces of data been returned.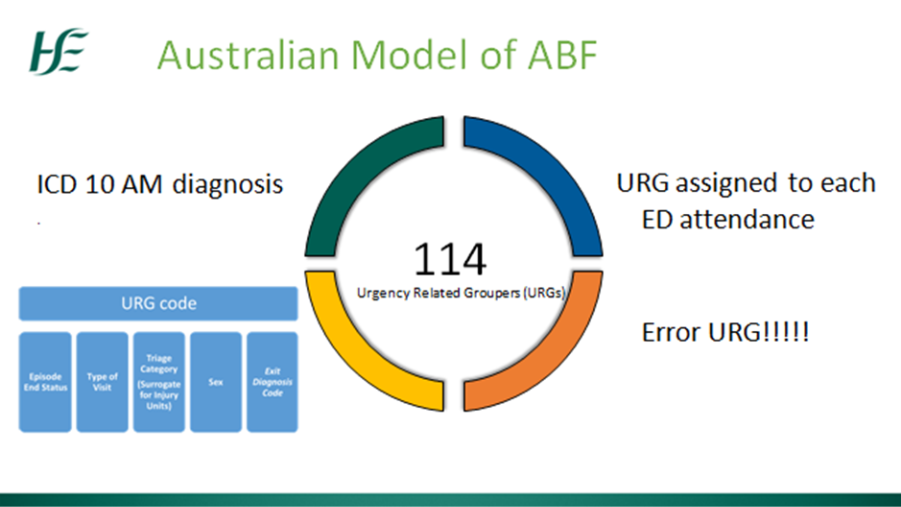
Every ED and Injury Unit has now been visited at least once and various means of facilitating the progression of this project have been employed outside of direct visits.
In terms of percentage compliance with coding of all attendances at EDs and Injury Units the following is the situation as of week ending 16th December:
*Almost all of the hospitals with a compliance level of 0% are upgrading or changing IT systems and have definite plans to commence coding in the near future.
The Healthcare Pricing Office is currently collecting and analysing the data as it is returned, to allow as comprehensive an analysis of activity as is possible. This will allow a URG to be assigned to each attendance with a diagnosis code, before proceeding to incorporate the URG with patient level costing for each hospital, with a view to proceeding to a period of shadow ABF funding, where each hospital will see the funding they would receive after the move from block funding to ABF.
|
Quality Improvement Project for Older Adults in Emergency Departments and Injury Units
Emergency Departments (EDs) and Injury Units are seeing a steady rise in attendances from older adults, with more than 560 people aged 75 and over presenting every day. To ensure that every older person receives safe, timely and respectful care, regardless of when or where they attend, a new national Quality Improvement Programme (QIP) has been developed.
Emergency Departments (EDs) and Injury Units are seeing a steady rise in attendances from older adults, with more than 560 people aged 75 and over presenting every day. To ensure that every older person receives safe, timely and respectful care, regardless of when or where they attend, a new national Quality Improvement Programme (QIP) has been developed.
The QIP is structured around three priority areas designed to standardise and strengthen care nationwide:
• Minimum Care Standards for Older Adults in EDs and Injury Units
• Post-Triage Assessment and Bundles of Care
• Education and Workforce Development
Older adults face unique risks in the emergency care environment, including functional decline, delayed assessment and increased vulnerability to delirium, frailty and falls. Many of these risks are not detected at standard triage. The QIP addresses this by promoting consistent minimum standards and introducing structured post-triage assessment bundles to ensure early identification and tailored care.
Key recommendations include avoiding MTS Category 5 triage for patients aged ≥75 unless clearly justified, reviewing Category 4 cases where uncertainty exists and embedding a post-triage assessment bundle for all older adults. This bundle incorporates the 4AT Delirium Screen, Clinical Frailty Scale, Falls Risk Assessment, Trauma Safety Net Checklist and a “What Matters to You” prompt-supporting more person-centred, age-attuned decision-making.
Developed in partnership with the National Emergency Medicine Programme and informed by teams across University Hospital Limerick, Sligo University Hospital, Beaumont Hospital, Cork University Hospital and St Vincent’s University Hospital, the QIP reflects a national shift toward needs-based, value-driven emergency care for older people.
The QIP is under review by the Chief Clinical Officer Forum and is expected to be launched in Q1 2026.
Emergency Medicine Early Warning System (EMEWS) Digitisation Project
The National Clinical Guideline for the Emergency Early Warning System (EMEWS) was launched in 2018. This was in response to growing concern and evidence (HIQA, 2012) that undifferentiated and undiagnosed patients were deteriorating in overcrowded Emergency Departments (EDs) in the time between triage and waiting for clinician assessment.
The National Clinical Guideline for the Emergency Early Warning System (EMEWS) was launched in 2018. This was in response to growing concern and evidence (HIQA, 2012) that undifferentiated and undiagnosed patients were deteriorating in overcrowded Emergency Departments (EDs) in the time between triage and waiting for clinician assessment. In October 2025, Bernard Gloster (HSE CEO) mandated the full implementation of EMEWS in all EDs nationally. This was in part fulfilment of Retired Chief Justice Clarke’s recommendations (September, 2024) to protect patients from harm. In consultation with ED nurses across the country, EMP is aware of issues in the day-to-day operationalisation of the EMEWS with the paper system.
The Emergency Medicine Programme (EMP) in collaboration with HSE Medical Device Equipment Management is advancing patient safety in Emergency Departments with the Digital Emergency Early Warning System (EMEWS). Following successful pilots at Mercy Hospital Cork and St. Vincent’s University Hospital Dublin in 2025, early feedback shows the Digital EMEWS) system improves timely observations, supports clinical escalation, reduces nurse workload and enhances collaboration between ED staff. Moving from paper to digital is expected to reduce errors, support audits and generate long-term cost savings. A national rollout is being considered, with the next steps including review of pilot reports, funding decisions and phased implementation across EDs.
Domestic, Sexual and Gender Based Violence (DSGBV)
A New Quality Improvement Framework to Strengthen DSGBV Identification and Response in EDs and Injury Units.
Emergency Departments (EDs) and Injury Units (IUs) are often the first point of contact for people experiencing Domestic, Sexual and Gender-Based Violence (DSGBV).
A New Quality Improvement Framework to Strengthen DSGBV Identification and Response in EDs and Injury Units
Emergency Departments (EDs) and Injury Units (IUs) are often the first point of contact for people experiencing Domestic, Sexual and Gender-Based Violence (DSGBV). While their immediate role is to treat urgent physical and psychological needs, these settings also offer a crucial opportunity to recognise hidden abuse and link patients with support.
A new Quality Improvement Framework has been developed to help frontline teams respond more confidently and consistently to DSGBV. Informed by national expertise, frontline experiences a national survey and pilot work across Irish sites, it provides practical, tiered guidance using a “Must Do, Should Do, Could Do” approach.
Among 151 respondents from EDs and IUs to a recent survey, including nurses, ANPs, consultants and medical social workers, only 31 reported having a designated DSGBV clinical lead. Fewer than 50 had a written protocol or clear referral pathway and social work support, while integral, was reported as significantly reduced after hours. Training gaps also emerged as a major challenge: 112 respondents cited lack of staff training and only 20 had received training in the last two years. Interest in national or regional DSGBV training initiatives was high however, with many staff keen to engage in structured learning.
Key priorities in the Framework include enhancing staff awareness, establishing local referral pathways, supporting evidence-based screening where feasible and aligning with already available tools and resources. The survey’s themes of limited protocols, inconsistent training, reduced out-of-hours supports and appetite for standardisation reinforce the importance of adopting a consistent, trauma-informed approach.
All EDs and IUs are encouraged to establish local DSGBV referral protocols, provide education and resources to staff, consider screening interventions where supported and track progress through simple quality measures. Developed in partnership with the National Emergency Medicine Programme and informed by pioneering clinical and social work teams across multiple hospitals, this Framework aims to strengthen safety, consistency and support for all patients affected by DSGBV.
The framework is under review by the Chief Clinical Officer Forum and is expected to be launched in Q1 2026.
|
|
National Emergency Department Triage Quality Improvement Framework (2025–2027)
Launched in September 2025, the framework marks one of the most significant reform efforts to the triage process in Irish Emergency Departments.
The National Emergency Department Triage Quality Improvement Framework (2025–2027) responds directly to long-standing concerns from frontline teams and key recommendations to the report by former Chief Justice Frank Clarke SC. Launched in September 2025, the framework marks one of the most significant reform efforts to the triage process in Irish Emergency Departments. At its core, the initiative aims to restore triage to its essential purpose: rapid, safe clinical prioritisation in an increasingly complex and crowded ED environment.

Over time, triage in many EDs has expanded beyond its original scope, with staff carrying out additional tasks such as administering medications, initiating investigations, or delivering analgesia. While well-intentioned, these activities have lengthened triage times and increased risks for undifferentiated, potentially deteriorating patients. The new framework refocuses triage on clinical risk assessment while building stronger pre- and post-triage systems to support patient flow.
The QIP outlines clear objectives across three phases of care. Pre-Triage initiatives include digital self-registration and rapid streaming pathways that divert suitable patients away from the ED, reducing congestion and time to triage. Triage itself will be reinstated as a fast, prioritisation-only step. In the Post-Triage phase, structured assessment and early interventions such as the Emergency Medicine Early Warning System (EMEWS) and rapid initiation of care bundles will accelerate diagnostics, decision-making and multidisciplinary involvement.
A major emphasis of the framework is transparency and accountability. Key Performance Indicators (KPIs) will be monitored weekly, with monthly reports to Health Regions, enabling real-time visibility of flow challenges and informing resource planning and staffing models.
The impact of these reforms is already evident. At St. Luke’s General Hospital Kilkenny, the pre-triage streaming of GP-referred patients has significantly reduced duplication of assessments and improved access to the Acute Medical Unit, Paediatric Assessment Unit and other specialist pathways. Staff report smoother workflows, enhanced safety and better patient experiences.
Looking ahead, national communications will launch in early 2026, with the first KPI benchmarking review scheduled for Q2. As this multi-year programme progresses, it represents a coordinated national commitment to safer, faster and more effective emergency care.
|
|
Children’s Emergency Medicine
The newly established Paediatric Unscheduled Care Steering Group convened in November for its inaugural meeting under the chairmanship of Ciara Martin. The group brings together representatives from regional hospitals, Children’s Health Ireland (CHI), nursing and medical staff with expertise in paediatrics and emergency medicine, as well as public health and patient interest representatives.
The newly established Paediatric Unscheduled Care Steering Group convened in November for its inaugural meeting under the chairmanship of Ciara Martin. The group brings together representatives from regional hospitals, Children’s Health Ireland (CHI), nursing and medical staff with expertise in paediatrics and emergency medicine, as well as public health and patient interest representatives.
At the meeting, the Steering Group formally reviewed and approved its Terms of Reference (ToRs), which outline its purpose: to enhance delivery of, and access to, unscheduled care services for children and young people, including those aged 16–17.
Updates from the working group highlighted ongoing mapping of children’s care pathways across 17 sites that treat both adults and children, as well as the presentation of a literature review by Dr. Sean Underwood. Plans are in place for a Focus Group in March 2026 as part of IPEM 2026, and data on paediatric admissions and PET data will be used to support the project.
Looking ahead, quarterly meetings have been scheduled to review progress and ensure alignment with the Steering Group’s strategic objectives. This collaborative effort aims to standardise paediatric emergency care, strengthen care pathways and ensure high-quality, equitable services for children across Ireland. By integrating insights from multiple disciplines and regions, the Steering Group is set to play a pivotal role in shaping the future of paediatric unscheduled care nationwide.
Other Events and Calls relating to Emergency Medicine
Global Emergency Care Skills Led Training (GECS)
More than sixty emergency care professionals at Solwezi General Hospital benefited from a week of intensive clinical skills training delivered by Global Emergency Care Skills (GECS). The initiative supported emergency and critical care develop
ment in Zambia’s Northwestern Province and highlighted the growing need for accessible high quality training resources, a need that is increasingly met through platforms such as SURGhub.

Interventional Trauma Simulation Study
Congratulations to Nikita Vainberg and the team in St. James's on the publication of their study
arising from the Interventional Trauma Simulation Study.

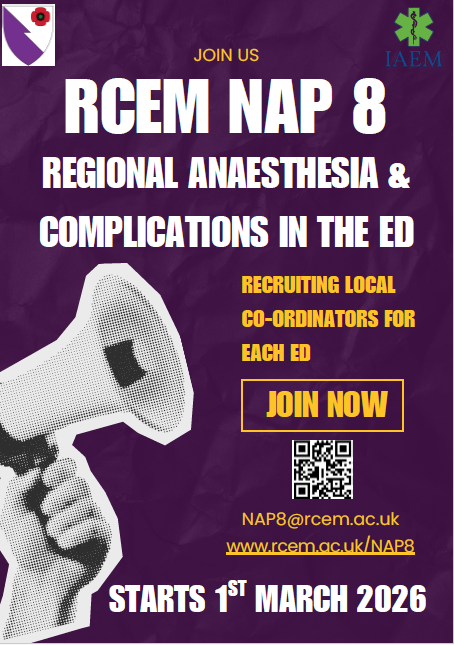
Call for NAP8 Local Coordinators
NAP8: Major Complications of Regional Anaesthesia is the first NAP project led by Emergency Medicine, delivered by RCEM, IAEM and RCoA. It will map current ED regional anaesthesia practice and complications to improve care and patient safety across the UK and Ireland. The project is due to go live on 1st March 2026.
Charter Day
The annual RCSI Clinical Programme Day at Charter Meeting will take place in RCSI on Wednesday, 11th February. Registration is free for the Wednesday event. Please email emp@rcsi.ie and we will notify you when registration is live.
Looking forward to 2026
For 2026, as well as continuing some of the above projects there are new streams and projects being developed. We plan to deliver a Quality Improvement Project on the management of older adults in the ED. We also plan to update guidance on DSGBV on ED/IU. If you have an idea or particular interest, please talk to the team and see how you can get involved.
All EMP Documents and Resources can be accessed on EMNOW.
If you have any feedback or require any information, please email emp@rcsi.ie
Wishing you all a Very Happy New Year for 2026
|
|
|